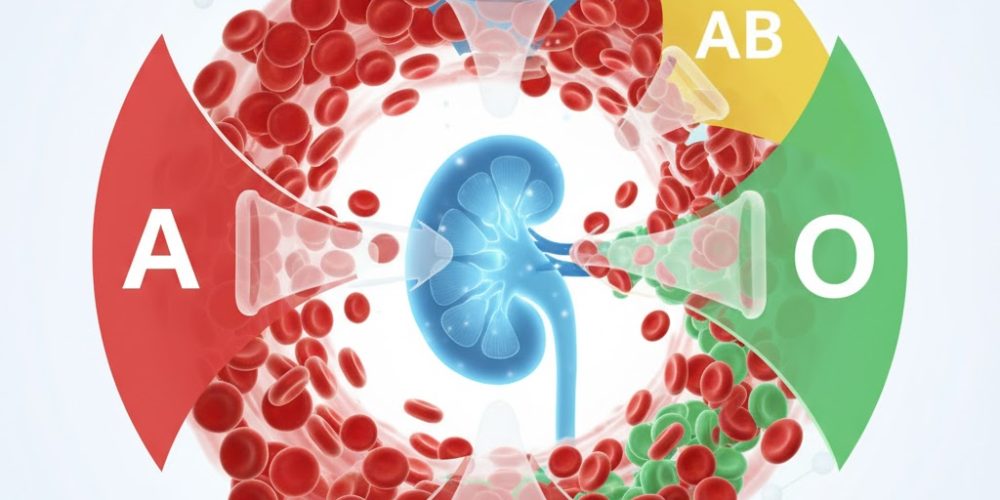
In a groundbreaking first, researchers have successfully converted a donor kidney from blood type A to blood type O before transplanting it — a breakthrough that could reshape transplantation for patients waiting with rarer blood types.
Blood type O recipients, who form more than half of those on kidney waiting lists, typically wait years longer for a match. That’s because O kidneys are universal donors, but usually given first to recipients with other blood types. The conversion addresses this mismatch by altering the organ itself rather than trying to suppress the recipient’s immune system.
Using specialized enzymes, scientists treated the donor kidney to remove antigens tied to its original blood group. In a first-in-human trial, the modified kidney was transplanted into a brain-dead recipient. The organ functioned without severe immune reaction for two days; by day three, a mild immune response appeared but was substantially less aggressive than expected in mismatched transplants.
“This is the first time we’ve seen this play out in a human model,” said Dr. Stephen Withers of the University of British Columbia, who co-led the enzyme development. He added that results provide crucial insight into how to refine the method for longer-term success.
Traditional approaches require patients to undergo intensive immunosuppression protocols for several days before transplant. This enzyme-based strategy avoids that, potentially lowering risks and opening up more donor-recipient matches.
Still, the path forward includes hurdles: the approach needs regulatory approval for clinical trials, validation of long-term outcomes, and confirmation that the technique is safe and reproducible for living patients.
If successful and widely adopted, this technique could shorten wait times, save lives, and revolutionize transplant medicine.